Now that I have published my blog, I have been approached by several people saying, “Why Fat Geriatrician? You aren’t Fat.” First of all, thank you for reading the blog! Second of all, thank you for your kindness–but I’ve got a BMI of 37.8. Objectively and according to the WHO, I am “Severely Obese.”
So, here is my attempt at explaining why the name Fat Geriatrician appealed to me.
Fat and Old are dirty words in our culture. We can still make fun of people who are fat and people who are old without really getting called out on it. People assume that someone who is fat is also lazy, unhygienic, and dumb. People assume that someone who is older is slow, feeble, and forgetful.
I see both groups as underdogs. People fighting to be seen as who they are and not the label that society puts on them. And boy let me tell you:

In the past few years I have come to own and embrace my size. I don’t care about it in a vain way. Once I embraced shopping in plus sized stores, I started jazzing up my look. I added dresses, bright colors, and makeup. I have never felt more fabulous or self-confident.
The only thing that worries me about my size is possible health consequences and early functional losses due to being overweight–hence starting an exercise program (see my first post).
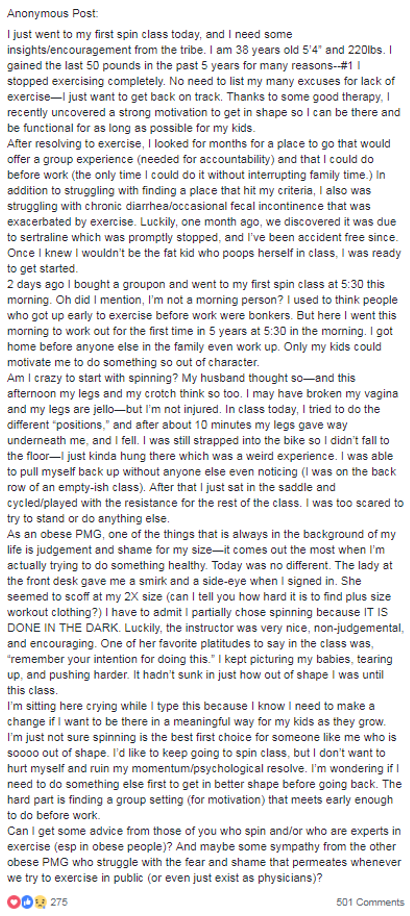
But many people who are fat are not able to embrace their size or practice self-love. Being obese is often complexly intertwined with other psycho-social issues.
The healthcare system can be especially judgmental (beyond health concerns) of fat people. We are (unfortunately) becoming a majority of patients. Medical school teaches cultural competency and has made judging certain diseases taboo (ex. HIV, alcoholism, depression). However, doctors can still openly judge and shame obese patients–and call it counseling.
I’m constantly getting the side-eye from other doctors (who don’t know me well) about my weight. I was shamed by attendings for my weight during my training. I’ve heard physicians and surgeons make snide comments about the weight of patients. And believe it or not, I was interviewing a trainee for a spot in one of our university’s training programs and this person had the nerve to give the bodycheck/eyeroll/snide remark trio to me about my weight. If this person did that in an interview, imagine what they would do to a vulnerable patient?
Despite popular opinion fat people are not dumb. We are actually highly attuned to this kind of behavior (I can say this as a member of the fat tribe).
There is research on weight discrimination in healthcare. It has been found that more than half of doctors describe their overweight patients as ugly, awkward, and noncompliant with treatment. Nearly one quarter of nurses admitted to feeling repulsed by their obese patients. Patients pick up on this and do not come back. My working hypothesis about “noncompliance” in many obese patients is that it has more to do with a poor doctor/patient alliance than anything intrinsic to the patient.

Hopefully I have convinced you that fat people are underdogs, especially in medicine. Now let me convince you about old people.
One of the things I love the most about being a geriatrician is I get to work with a patient population who is not used to being seen or valued. They are under-served, but not even on the healthcare system’s radar as being under-served because “50% of Hospital Length of Stay Days are for people age 65+.” Access and appropriate care are not the same thing.
Anti-Ageism Rant:
Ageism is one of the only acceptable “-isms” left in America, and it is alive and well in the healthcare world.
I can’t tell you how many physicians have told me that they are experts in taking care of older adults (despite no training in aging) because they do it all the time? The problem is they don’t do it well, and they don’t know it can be done better. Older adults can also be ageist against themselves in a healthcare system–insisting that their symptoms are due to age. They also rarely want to admit that they are older adults and that they could benefit from the expertise of someone in geriatrics. We have a branding problem in our field.
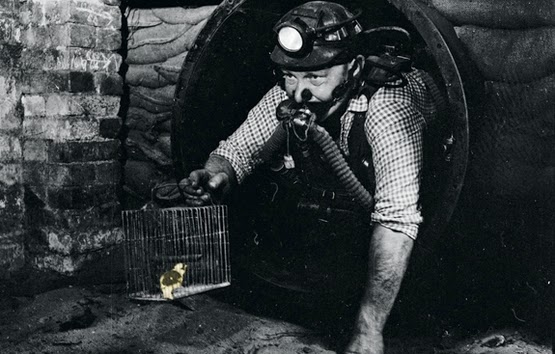
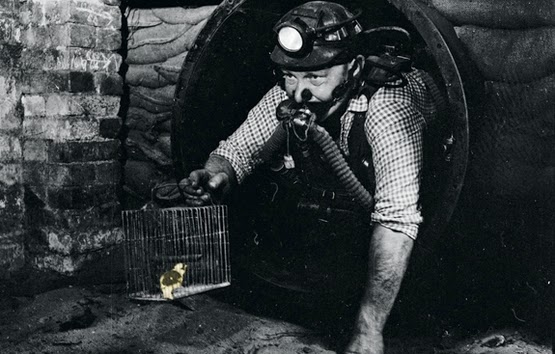
One of my geriatric idols/attendings used to say “Older adults are the canaries in the coal mine for healthcare.” He was so right. As we age we become more vulnerable, and our fractured healthcare system that has been set-up for middle aged adults can be downright dangerous for older adults. When something can go wrong in healthcare, it will go wrong for our older adult patients first.
So I have embraced a career of taking care of these underdogs and their caregivers. It is more fulfilling than you could ever imagine to see someone who has been told, “oh you are just wetting yourself/forgetful/falling/etc because you are old,” and then making them dry/think clearly/stop falling by practicing good geriatric medicine. It is life changing for the patient, and brings me so much joy as a doctor.
I also love geriatrics because we fear weight loss. It is a harbinger of functional loss and declining health. So I got to stop having the uncomfortable you need to lose weight discussions with patients who weighed less than I did. Instead I get to give the “you can ditch your low salt, low carb, low fat diet–just please eat,” talks! They are much easier for me as a fat doctor.

I think that being a fat “underdog,” and experiencing hidden prejudice in the healthcare system myself is a big part of what drew me to the field of geriatrics. And therefore, it seemed very fitting to put these two ideas together in the name of my blog.
So there you have it! Fat Geriatrician for the Win!